Summary: Periodontal disease is a significant public health concern that affects millions globally. Understanding its management strategies is critical for improving oral health and overall wellbeing in patients. This article explores four key strategies: early diagnosis, personalized treatment plans, patient education and engagement, and regular follow-up care. By examining these aspects, healthcare providers can enhance treatment effectiveness, foster better patient compliance, and ultimately lead to improved health outcomes. The need for a multi-faceted approach to periodontal disease management is emphasized, as it impacts not just oral health, but overall quality of life.
1. Importance of Early Diagnosis and Intervention
Early diagnosis of periodontal disease is crucial to prevent its progression and associated complications. Routine dental check-ups allow for the identification of gingival inflammation and attachment loss in their initial stages. A proactive approach helps mitigate the risks associated with advanced periodontal disease, which may lead to tooth loss and systemic health issues.
Diagnostic tools, such as clinical examinations and radiographs, play a vital role in determining the extent of periodontal disease. Dentists can accurately assess pocket depths, attachment levels, and bone loss, enabling timely interventions. The use of screening questionnaires can also enhance early detection, making it necessary for practitioners to incorporate them during patient visits.
The importance of regular dental visits for at-risk populations, such as smokers and diabetics, cannot be understated. By recognizing high-risk groups and scheduling frequent assessments, healthcare providers can facilitate early treatment that effectively improves long-term outcomes.
2. Creating Personalized Treatment Plans for Patients
Personalized treatment plans are essential for effective management of periodontal disease. Each patient’s condition varies widely, necessitating tailored approaches that consider individual oral health status, lifestyle factors, and patient preferences. Collecting comprehensive information during the initial consultation allows dental professionals to develop an effective and realistic treatment plan.
Factors such as the patients age, general health, and specific bacteria present in their mouth significantly influence how periodontal disease should be treated. For example, younger patients may benefit from more aggressive treatments, while older individuals might require gentler approaches. Taking these aspects into account ensures that treatments are both effective and sustainable.
Moreover, incorporating a collaborative decision-making process fosters patient autonomy and encourages adherence to the prescribed treatments. A personalized plan that emphasizes the patients role in their oral health journey is key to achieving lasting results.
3. The Role of Patient Education and Engagement
Patient education plays a significant role in managing periodontal disease. Empowering patients with knowledge about their condition enables them to take active roles in their oral health. Educational initiatives should cover topics such as proper brushing and flossing techniques, the importance of regular dental cleanings, and understanding the risk factors associated with periodontal disease.
Moreover, utilizing various resources, including brochures, online materials, and interactive demonstrations, can effectively enhance patient engagement. These methods help patients assimilate information better and encourage them to ask questions, leading to increased understanding and compliance with treatment.
Engaging patients in their treatment plans is also crucial for fostering accountability. Regular check-ins, personalized follow-up calls, and interactive sessions can motivate patients to remain committed to their oral hygiene practices. By establishing a partnership between the dental provider and the patient, healthcare professionals can significantly improve treatment outcomes.
4. Importance of Regular Follow-Up Care
Regular follow-up care serves as the backbone of effective periodontal disease management. Just as initial treatment is vital, ongoing assessment and maintenance are essential to preventing disease recurrence and progression. Scheduled follow-ups enable dental professionals to monitor the patients health, adjust treatment plans, and provide necessary interventions, ensuring long-term success.
During follow-up visits, dental professionals can conduct periodontal evaluations, including probing for pocket depths and assessing gingival health. These assessments help identify any changes in the patient’s condition, informing the need for additional treatments or adjustments. Furthermore, follow-up care reinforces the importance of sustained oral hygiene practices between visits.
Moreover, successful management of periodontal disease includes fostering a supportive environment where patients feel comfortable discussing their challenges. Regular follow-ups pave the way for open communication, allowing patients to express their concerns and report obstacles they might be facing in adhering to their oral care plans.
Summary: The management of periodontal disease is a multi-faceted endeavor that requires early diagnosis, personalized treatment plans, patient education, and regular follow-up care. These strategies not only improve oral health but also contribute positively to overall wellbeing. A collaborative approach between healthcare providers and patients is essential for achieving the best outcomes.
This article is compiled by Vickong Dental and the content is for reference only.
Vickong Dental
Vickong Dental is a large medical group established in Hong Kong in 2008 by professors from well-known medical universities in Guangdong and Hong Kong, as well as medical doctors from key national '985' universities (including Master's supervisors and senior professors). The chain of branches brings together expert dentists with PhDs and Master's degrees from Hong Kong and Mainland China, committed to providing high-quality dental treatment.
"Vickong Dental Practices the University Motto of 'Healing and Serving Society,' with a Stable Operation for Sixteen Years. It Has Been honored with Hong Kong Enterprise Leaders's Choice,' and is a Global Trusted Implant Center for the Nobel Implant System. Recommended by Hong Kong Metro Broadcast and Guangdong Television, it Serves Customers from Over Thirty Countries and Regions, Gaining the Trust and Favor of Citizens from the Guangdong-Hong Kong-Macau Greater Bay Area and Surrounding Cities.

Thousands of customers' unanimous praise
The most recognized and highly recommended dental service by customers in the Guangdong-Hong Kong-Macau Greater Bay Area
We Ensure You Receive Detailed Care and Attention Here
Hong Kong standards, Shenzhen prices, Your Trusted English-speaking dentists

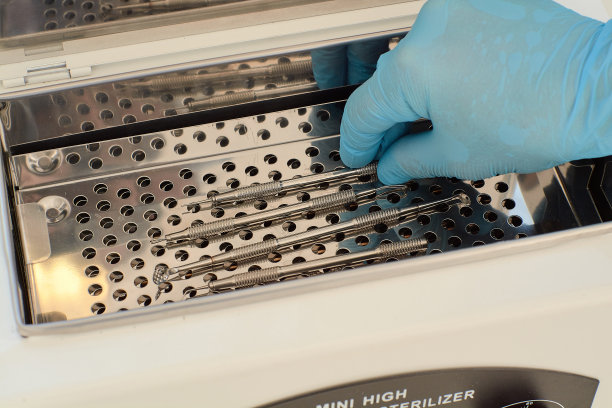
Vickong Dental Medical-Grade Instrument Disinfection Process
Vickong Dental Medical-Grade Instrument Disinfection Process

Vickong Dental Chain: A Warm and Comfortable Environment for Treatment






Appointment Hours

Q&A
Why choose Vickong Dental?
Vickong Dental practices the university motto 「Medicine to Benefit Society」, with each branch bringing together highly qualified dentists with doctoral and master’s degrees from Hong Kong and the Mainland, and has maintained seventeen years of steady operation。Recipient of 「2024 Hong Kong Enterprise Leaders Brand」, 「2025 Hong Kong Enterprise Leaders Brand」, a Nobel Biocare Global Trusted Implant Center, and a brand recommended by Metro Radio Hong Kong and Guangdong TV。
To date, we have served customers from more than thirty countries and regions,earning exceptionally high word-of-mouth recognition and trusted recommendations from residents across the Guangdong-Hong Kong-Macao Greater Bay Area and surrounding cities
We have eight major branches in Zhuhai、Shenzhen,and a consultation and service assurance center in Hong Kong,so you can book a free consultation at any time for any questions,which is very reassuring.
If I do not accept the quotation after the CT scan, will I be charged??
No! As long as the actual treatment has not started, you will not be charged any fees.
Will there be any additional charges during the treatment process?
No, there won’t be any additional charges. Before treatment begins, we will clearly explain the treatment plan and its corresponding fees. Only after the patient agrees and signs the consent form will we proceed with the dental service.
Can I pay in Hong Kong dollars?
Yes. Vickong Dental accepts payment in Hong Kong dollars. The amount will be converted based on the exchange rate of the day, and the applicable rate will be clearly communicated to you in advance.
Can I reschedule my appointment at any time?
Yes. Please contact us via **WeChat** or **WhatsApp** as early as possible, providing your original appointment time and details, along with your preferred new date and time slot for rescheduling.













